
Streamlining independent medical review processes for digital transformation
Key takeaways
The COVID-19 pandemic dramatically increased the volume and types of medical coverage appeals submitted to qualified independent contractors (QICs) for reconsideration on behalf of the Centers for Medicare and Medicaid Services (CMS). In response, long-trusted CMS partner Maximus leveraged robust processes and leading technologies to streamline independent medical reviews, increase efficiencies, and improve quality at scale.
Leveraging advanced technologies to improve process efficiencies
Situation
To expand coverage and improve outcomes, CMS retains QICs staffed with medical professionals to provide independent reviews of appeals, reconsidering denials of coverage for beneficiaries. Maximus has served as the Independent Review Entity for the program since 1987, providing 2M+ decisions. With higher case volumes during the pandemic, CMS enacted program changes with significant impacts on the appeals process. In particular, more expedited-status appeals, which required process completion within 72 hours, were permitted.
Challenge
Appeal volumes increased from 17% to nearly 30% of cases, and the number of appeals requiring medical review (a costly element of the process) grew from 20% to 35% of reconsiderations. CMS needed to scale its review processes while controlling costs and maintaining compliance and quality.
Solution
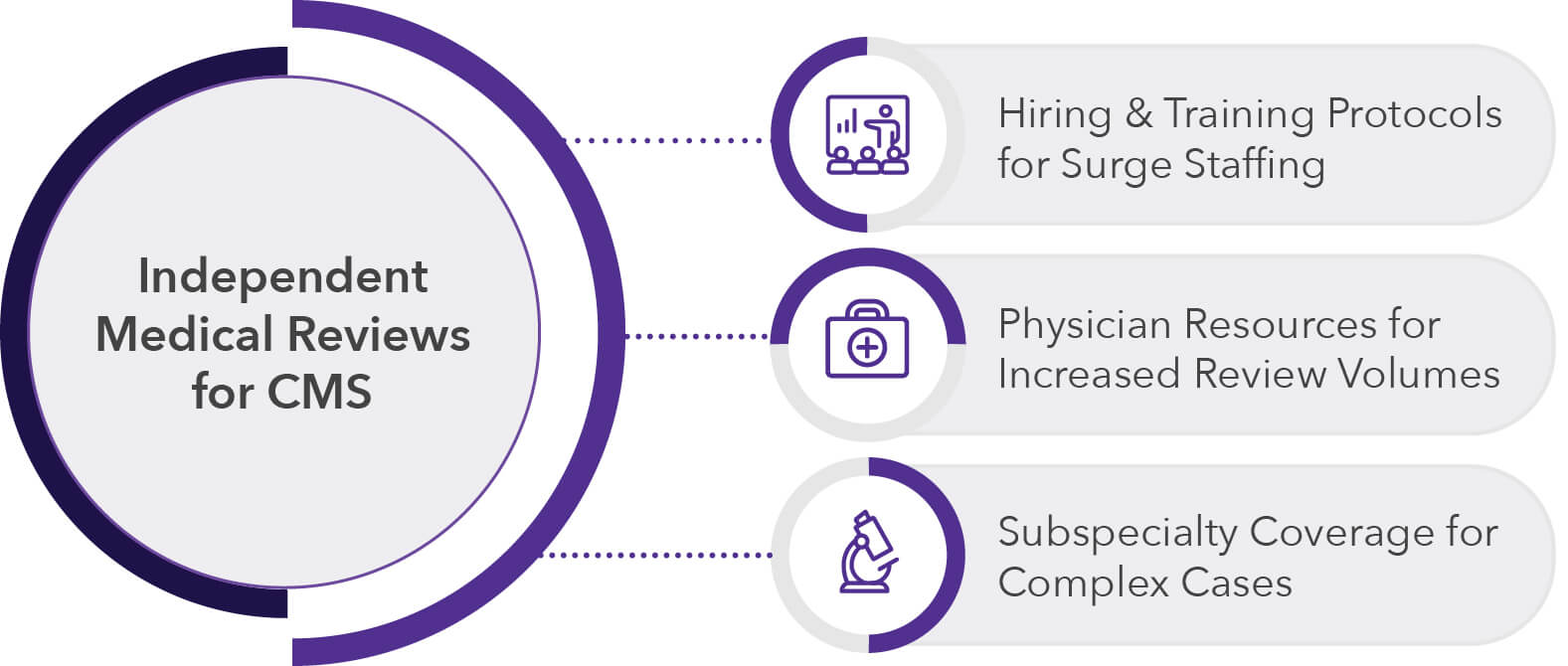
Leveraging more than three decades of experience rendering fast, independent, accurate determination of benefits from trained health professionals, Maximus was able to tackle these challenges for CMS by:
- Developing a hiring and training protocol to ensure proper staffing for increasing case volume
- Promoting internal staff into adjudication roles and providing employees with opportunities to move up within the project
- Adding physician resources to assist with increased medical review volumes
- Sourcing and bolstering additional physician panel resources
- Offering subspecialty coverage for increasing volumes of medically complex cases
How we did it
Maximus provided CMS with trusted expertise in hiring and training as well as case creation, closing, compliance, and quality control. Our team provided strategic technologies, including robotic process automation and methodologies, to streamline independent medical review processes and increase efficiencies.
Results
- Improved Independent Medical Review Process efficiencies
- Earned exceptional CPAR scores, including near-perfect quality and timeliness ratings
- Zero appeals accuracy issues identified by the CMS auditor
- Exceeded CMS leadership expectations amid a public health emergency
As a trusted technology and solutions service partner of CMS, Maximus is proud to support the advancement of the nation’s critical health needs, transform clinical care, and establish a blueprint for the future of public health.