Challenge
When the state faced increased applications for Medicaid, the Children’s Health Insurance Program (CHIP), the Supplemental Nutrition Assistance Program (SNAP), and Temporary Assistance for Needy Families (TANF), the volume of work for program eligibility workers also increased substantially. This put additional demands on the workers and increased application processing times. The Texas Health and Human Services Commission (HHSC) identified that a large-scale, integrated eligibility solution would enhance operational performance and streamline the application process for Texans seeking these benefits.
Solution
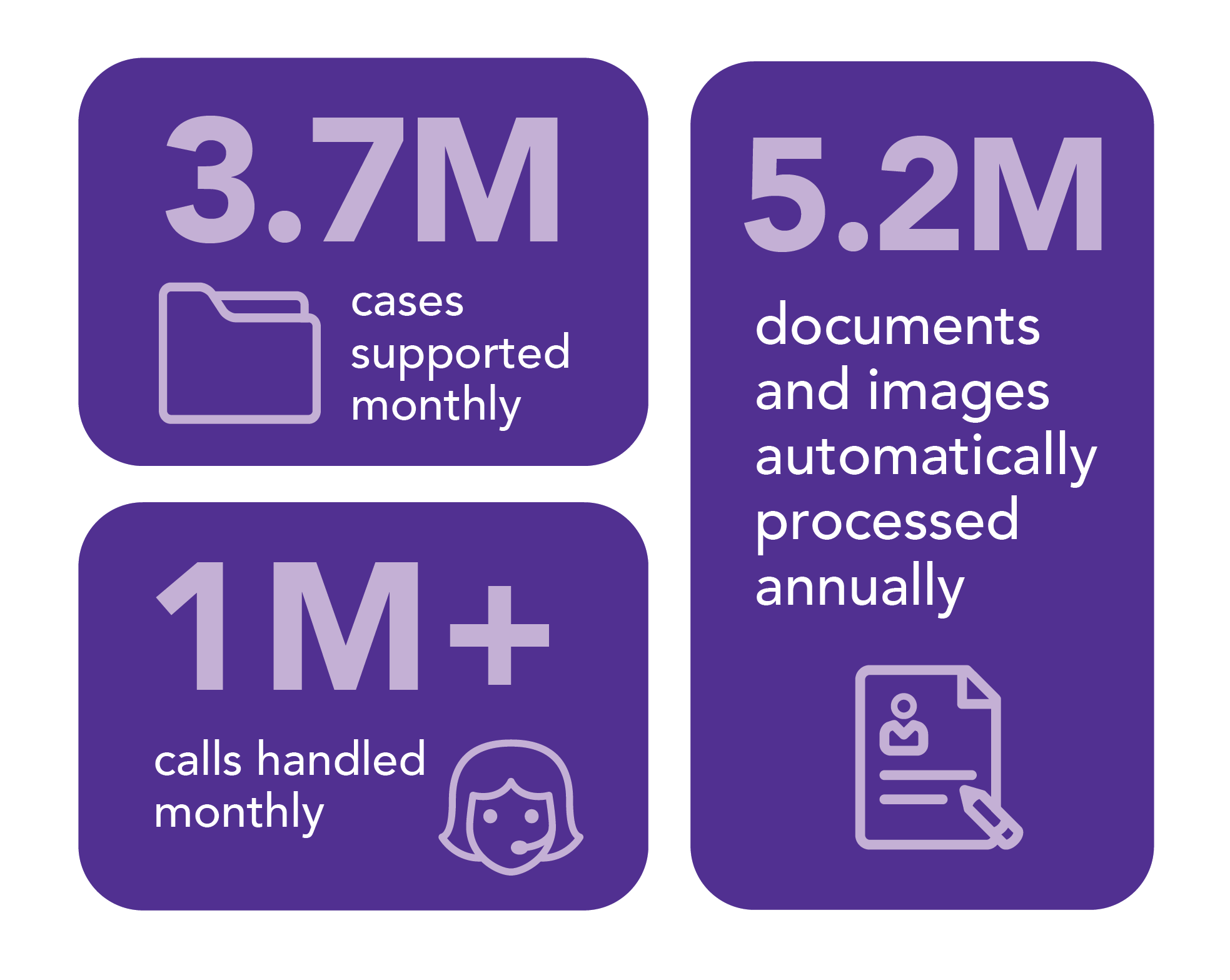
HHSC launched an integrated application and eligibility process for dozens of public assistance programs, including Medicaid, CHIP, SNAP, and TANF. In addition to introducing greater operational efficiencies, HHSC wanted to improve customer experience. HHSC selected Maximus to initially process the application documents and then send them to state employees to make final eligibility determinations based on standards set by the federal government and state legislature. HHSC also selected us to operate a customer contact center to help people navigate the eligibility process and answer their case or application questions.
How we did it
Working collaboratively with HHSC, we evaluated over 2,000 processes and helped the state consolidate support services for Medicaid, CHIP, SNAP, and TANF from county-based to statewide. This significantly improved performance by standardizing fundamental services, integrating the process of applying for and determining eligibility, and providing entry through multiple channels and self-service options.
- Self-service options: While continuing to deliver our core contact center and application support services, we implemented the state’s “self-service first” model in 2007. Today, online application submissions reduce the need for mail and paper document processing services. Callers use self-service interactive voice response technology to check their benefit status, receipt of supporting documents, appointment dates/times, and more, allowing our contact center agents to help other customers with more complex requests.
- Multichannel outreach: Recognizing the need for more than a one-size-fits-all approach, we implemented multichannel outreach — phone calls, text, email, and paper mail — to remind Texans to update their demographic information so the HHSC team can easily reach them when processing their cases. For those who prefer to interact by regular mail, we even introduced eye-catching yellow envelopes to help increase response rates to HHSC’s mailed communications.