Family caregivers and professional direct care workers, including personal care aides, home health aides, nursing assistants, and personal care attendants, assist older adults and people with disabilities daily. An estimated 70 percent of caregivers deal with stress in their daily lives. Specifically, AARP found that nearly 40 percent of caregivers said they “rarely” or “never” feel relaxed, which can lead to burnout.
Direct care workers and family caregivers support basic tasks like dressing, bathing, and eating. They also help with housekeeping, employment, or social engagements. According to a 2024 report, healthcare coordination, such as securing appointments and finding appropriate doctors, are some of the top sources of stress for caregivers. Also noted was getting relief help to find time for a break.
As America's population ages, these roles are becoming even more essential. Census projections estimate the population of Americans 65 and over will grow from about 15 percent today to over 20 percent by 2030 and nearly 25 percent by 2060, increasing demand for long-term services and support. Likewise, the Health Resources and Services Administration estimates that the number of caregivers will almost double by 2036.
Listen to caregivers
As assessment professionals, how can we help support caregivers? We can start by listening.
When my clinical services colleagues deliver person-centered assessments, we determine the services and supports individuals need to live safely at home, in the community, or in an appropriate institutional setting. Sometimes, caregivers are part of the process. They may be present as family members, authorized representatives, or even translators. And often, caregivers are among those who will provide the services and support we’ve identified. Through our interactions with caregivers, we take the time to listen when they share how their work is rewarding but also challenging.
Some caregivers experience heightened stress due to emotional factors, including compassion fatigue. Naturally, people feel compassion and empathy for others, but caregivers who face these emotions more intensely or for extended periods of time may develop physical, emotional, or psychological stress responses. Secondary trauma, the emotional duress that can happen when a caregiver hears about or witnesses the person, they are caring for experiencing trauma, can also occur.
The impacts of stress and trauma can lead to the more significant issue of burnout, where caregivers feel complete mental, physical, and emotional exhaustion. The National Institutes of Health describe burnout in this context as “a common syndrome observed in healthcare workers, defined as the combination of emotional exhaustion, depersonalization and a reduction in personal achievement, caused by chronic occupational stress.”
Encourage caregivers to embrace self-care
Around this time last year, Maximus participated in a training session for direct care workers, Building Your Self-care Toolkit, to support an initiative with the Colorado Department of Health Care and Policy Financing and the Direct Care Workforce Collaborative.
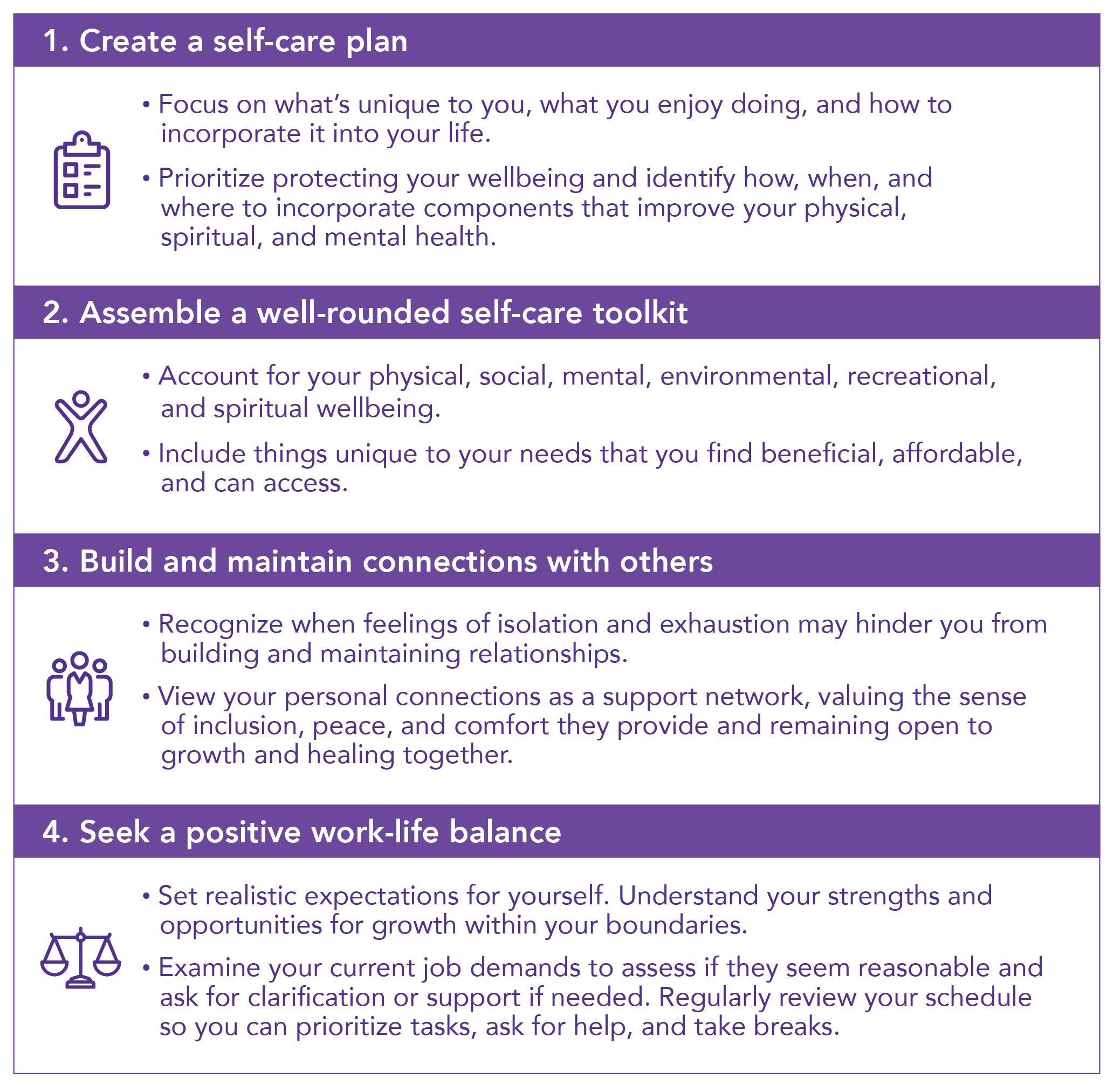
While there is no “one-size-fits-all” approach to self-care, it’s important to identify relaxing and enjoyable activities and maintain connections with others.
Here are a few tips that we shared with caregivers.